Lupine Publishers | Levonorgestrel Intrauterine System Effects Versus Copper Intrauterine Device on Changing of Menstruation and Uterine Artery Doppler
Lupine Publishers | Interventions in Gynecology and Women's Healthcare
Abstract
Background: The most effective methods for birth control are the long-acting reversible contraceptives LARCs include Paragard IUD in silver, Mirena IUD in hormonal (progesterone) and hormonal contraceptive implant. The intrauterine levonorgestrelreleasing system (LNG‐IUS) and the intrauterine copper unit (Cu‐IUD) influenced changing of menstruation and uterine artery Doppler indices.
Aim of the work: Comparison of the effects of copper intrauterine device (Cu‐IUD) and an intrauterine levonorgestrel releasing system (LNG‐IUS) on changing of menstruation and Doppler indices of uterine arteries.
Methods: This was RCT was completed between February 2017 to January 2020 at the Obstetrics and Gynecology department, Tanta University hospitals. There were two group first group A: LNG‐IUS (N=200) and second group B Cu‐IUD (N=200), they were randomly assigned to 400 multiparous women preferring intrauterine contraception., the UA pulsatility index (PI) and the resistant index (RI) were determined at the beginning, and the associations with irregular bleeding were evaluated three and six months after insertion
Results: In group A: LNG‐ IUS, some women registered irregular bleeding (28 percent) than in the Cu‐IUD group (52 percent) at the beginning of the study (P<0.001). There was bleeding irregularity (73 percent) in the group(A): LNG‐IUS and severe menstrual bleeding (68 percent) in the Cu‐IUD group. The uterine artery PI was associated with bleeding irregularity at value of 1.40, with a curve area (AUC) of 0.91, 90 percent sensitivity, and 100 percent specificity. Uterine artery RI was associated with 0.65 with 0.22 AUC bleeding irregularity, 95 percent sensitivity and accuracy 100 percent.
Conclusion: LNG‐ IUS related irregular bleeding was linked to changes in the blood flow of uterine arteries that were not evident among Cu‐IUD users.
Keywords:Intrauterine devices; LNG-IUS; cu-IUD, Long-acting reversible contraception; ultrasonography; Doppler; Color; Power Doppler
Introduction
Long acting reversible contraceptives (LARCs) are the most effective methods
for regulating birth. LARCs include silver Paragard IUD, hormonal Mirena IUD
(progesterone), and hormonal implant contraceptive. Such birth control methods
can prevent unwanted pregnancies up to 20 times better than birth control
pills, patches and vaginal rings [1].
The intrauterine levonorgestrel releasing system (LNG-IUS) has demonstrated its
effectiveness both as a long acting contraceptive and for its non-contraceptive
advantages, including high efficacy in the treatment of severe menstrual
bleeding. However, twentytwo and sixty seven percent of women had persistent or
repeated bleeding in the first months after placement, which decreased by first
year ending [2].
On the other hand, was associated with an increase of 30% to 50% in menstrual
blood loss and about 10% to 20% in users requesting withdrawal by first year
ending of use [3]. While some studies have indicated that the LNG‐IUS raises
the Doppler UA index three months after use due to an increased blood flow
impedance in the uterine arteries, [4-5] Others found no changes in the
Pulsatility Index (PI) or Resistance Index (RI) of the uterine artery between
LNG‐IUS users three months after insertion [6-7]. Similarly, studies of the
indices of uterine artery Doppler reported contradictory results to identify
the association between use of Cu‐IUD and heavy menstrual bleeding [8-9].
Knowing changes in the uterine vasculature among IUD users is important both in
terms of physiological and pathophysiological changes to help inform women
about their contraceptive choices [5]. The purpose of this study was to assess
the impact of LNG‐IUS versus Cu‐IUD on menstrual changes and Doppler uterine
artery indices 3 and 6 months after use.
Materials and Methods
The latest randomized clinical trial among new users of IUD was performed
between January 2017 to August 2019 at the Obstetrics and Gynecology
department, Tanta University hospitals. The study procedure had been accepted
by the ethical review committee of the Faculty of Medicine, Tanta University.
The study included multiparous women attending a normal menstrual cycle at the
family planning clinic who requested long acting reversible contraception and
met the intrauterine contraception criteria after providing a complete history
and undergoing clinical examination and transvaginal ultrasonography. Criteria
is omitted: Nulliparity, pregnancy, previous month’s genital infection,
undiagnosed uterine bleeding, medical conditions and any contraindications to
progestin administration or IUD insertion. Participants were assigned to one of
two classes by using computergenerated simple random tables. Women received
group 1 LNG‐IUS (Mirena, Bayer HealthCare, Berlin, Germany); women received
group 2 copper T‐380 IUD (Copper IUD, DPK, Egypt). Blinding was not done due to
the clear distinction between the two forms of IUDs. Uterine artery Doppler was
conducted in the Department of Radiology with a 7-MHz transvaginal probe and an
EUB‐7000 ultrasound instrument (Hitachi, Tokyo, Japan) prior to insertion of
the contraceptive tool, and three and six months after insertion. For avoiding
interobserver volatility.
The primary outcome measures were menstrual changes and improvements in the
three- and six-months following application of uterine artery Doppler indices.
In order to evaluate the correlation between uterine artery Doppler indices and
subsequent regular or serious menstrual bleeding, a regression analysis
included all women affected by an excessive bleeding at the three-and sixmonths
follow-up. The secondary results were side effects, and female
satisfactoriness.
Women were given calendars of menstruation to chart the days they suffered
bleeding the WHO suggested. The menstrual segment included both a bleeding
episode, and a bleeding-free cycle. Vaginal spotting was defined as very slight
bleeding which did not require sanitary protection, while heavy bleeding was
defined as hemorrhage which required sanitation. Analysis on side effects was
done with appropriate managing of stated symptoms at each scheduled visit.
Statistical analysis
Data entry, processing and statistical analysis was carried out using
MedCalc ver. 18.2.1 (MedCalc, Ostend, Belgium). Tests of significance
(Kruskal-Wallis, Wilcoxon’s, Chi square, logistic regression analysis, and
Spearman’s correlation) were used. Data were presented and suitable analysis
was done according to the type of data (parametric and non-parametric) obtained
for each variable. P-values less than 0.05 (5%) was considered to be
statistically significant.
To evaluate predictors of bleeding irregularity, multiple logistic regression
was used. The feature of the receiver operator (ROC) curve analysis was used to
determine the optimal cutoff value and sensitivity, and PI and RI specificity
to predict bleeding. A P value less than 0.05 has been found statistically
significant. The confidence interval was set at 95% and the accepted error
margin was set at 5%. So, at the level of < 0.05, the p-value was considered
significant.
Results
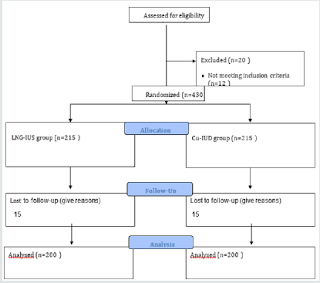
Overall, 450 females met the study criteria and were employed into the clinical trial. Of these, the 6-month follow-up study was attended and completed by 400 women (LNG‐IUS group, n=200; Cu‐IUD group, n=200) (Figure 1 & Table 1).
Figure 1: Consort flow diagram.
Table 1: The sociodemographic characteristics among studied groups.
Figure 2 & Table 2 showing that there was high statistically significant difference between two groups regarding side effects and acceptability of females two wards the contraceptive methods (P<0.001). at the beginning of the study, In LNG‐IUS group fewer females had irregular bleeding (28 percent) than in the Cu‐IUD group (52 percent). The bleeding was primarily in the form of irregular bleeding (73 percent) in the LNG‐IUS community and extreme menstrual bleeding (68 percent) in the Cu‐IUD group among those who had abnormal bleeding. The number of women experiencing irregular bleeding was down at six months in both groups. Also, there was high statistically significant difference between two groups regarding overall satisfaction (p<0.05) (Figure 3 Table 3).
Figure 2: Mean age of the studied group.
Figure 3: The side effects of contraceptive procedures in the studied groups.
Table 2: The adverse effects and women acceptability of the contraceptive methods.
Table 3: Comparison between the studied groups regarding Uterine artery pulsatility index.
Table 4 showing that there were significantly different regarding the first
PI (P<0.001) and RI (P<0.001) were of which were higher among women in
the LNG‐IU group. Also, both groups at three and six months, that there were
significantly different regarding PI and RI with the first Doppler indices (all
P<0.001).
The ROC curve study associated uterine artery PI with irregular bleeding at a
cutoff value of 1.40 with a curve area (AUC) of 0.91, 90 percent sensitivity,
and 100 percent accuracy. Uterine artery RI was associated with 0.65 with 0.22
AUC bleeding irregularity, 95 percent sensitivity& accuracy. 100 percent
(Figure 4 & Table 4).
Figure 4: ROC curve analysis of the relationship between pulsatility index (PI) and resistance index (RI) of an irregular bleeding and uterine arteries.
Table 4: Comparison between the studied groups regarding Uterine artery resistance index by study group.
Table 5 showing that Multiple logistic regression analysis of bleeding abnormality and female features shown a significant correlation between uterine artery PI and RI at baseline (P<0.001).
Table 5: Multiple logistic regression analysis of bleeding abnormality and female features.
Table 6: ROC curve analysis of uterine artery Doppler indices to predict abnormal bleeding.
Discussion
Long acting reversible contraception (LARC) methods such as intrauterine
levonorgestrel releasing (LNGIUS) are safe and highly effective in preventing
pregnancy. Previous studies had been done Doppler indices of the uterine artery
and correlate with menstrual abnormalities reported conflicting results [4-6].
Women that use LNG-IUS will experience excessive or unusual bleeding in the
first months following placement, as reported by 22% and 67% of users,
respectively, and this abnormal bleeding will decrease by the end of the first
year [2]. As expected, in this study, women using LNG-IUS reported lower rates
of menstrual disorders and greater acceptability compared to cu-IUD, which
could be largely attributed to menstrual irregularities and fear of declining
future fertility. Women using LNG-IUS experienced greater acceptability in
terms of overall satisfaction (p<0.001) and method recommendation to other
women (p<0.05). In the current study, excessive uterine bleeding has been
shown to be positively associated with hemodynamic changes in the uterine
artery, with a significant decline in PI and RI among new users of LNG‐IUS but
not Cu‐IUD.
Jiménez et al. [5] LNG‐IUS first recorded positive effect on uterine artery PI.
It was found that LNG‐IUS was independently associated with increased uterine
artery PI among 27 women after age and parity control, whereas in a study
evaluating PI just before mid-luteal insertion and three months after insertion
there was no difference among 25 women receiving TCU 380A IUD. Recently, more
so. Similarly, Järvelä et al. [4] Who in 13 postmenopausal symptomatic women
who obtained transdermal estradiol 1 month before combining LNG‐IUS with
replacement estrogen therapy measured uterine PI. The same group subsequently
stated in a study of 27 healthy, regularly menstruating women that LNG‐IUS
injection in the mid-luteal phase in combination with serum LNG and associated
decrease in serum progesterone tended to increase impedance to the uterine
arterial blood flow Another longitudinal study Conducted by Bastianelli et al.
[6] concluded that LNG‐IUS not only altered endometrial thickness but also
significantly altered uterine blood flow among women with excessive bleeding,
Zalel et al. [10] After insertion of LNG‐IUS in 47 women and insertion of Cu‐
IUD in 35 women, no changes in blood flow in the uterine artery were identified
when measured prior to and after use. Dane et al. [11] Reduced sub endometrial
vascularization and higher spiral artery uterine PI among 25 new users of
Depo-medroxyprogesterone acetate injection but no improvements among 25 new
LNG‐IUS users.
More recently, Cihangir et al. [7] reported that there was no significant
change in the volume of ovaries or uterine RI and PI at 6 or 12 months with
respect to the pre-insertion values among 49 users of LNG‐IUS. Regarding the
Cu‐IUD, recent studies identified a lack of significant changes in the uterine
artery’s PI and RI with or without side effects, including dysmenorrhea, heavy
menstruation and dyspareunia, 3 or 6 months after insert. [5,9-12] high menstrual
bleeding associated with the Cu‐IUD could be due to the mediated development of
vasoactive agents other than prostaglandins in the surrounding tissue [13]. The
differences among the above studies may be due to the small sample sizes, or
the measurement of Doppler indices at specific menstrual cycle periods or times
of the day, or by various ultra-sonographers. Such contradictory variables had
been omitted in the current study. Indeed, the design of the study and the
greater number of participants form the main strengths of the study [14].
Regarding the study’s weaknesses. no extension of the duration of follow-up or
comparison of other longacting contraceptive methods was needed.
Conclusion
In conclusion, LNG‐IUS-related irregular bleeding was linked to changes in blood flow to the uterine artery that were not apparent among Cu‐IUD users. Uterine artery Doppler is an easy, affordable, and readily available method for diagnosing women with irregular uterine bleeding after insertion of the LNG‐IUS for contraception. Future research will focus among new users of Cu‐IUD on the predictive value of Doppler indices on the uterine artery and subsequent heavy menstruation.
Read More Lupine Publishers Gynecology Journal Articles: https://lupinepublishers-gynecology.blogspot.com/


Comments
Post a Comment